Image via Wikipedia
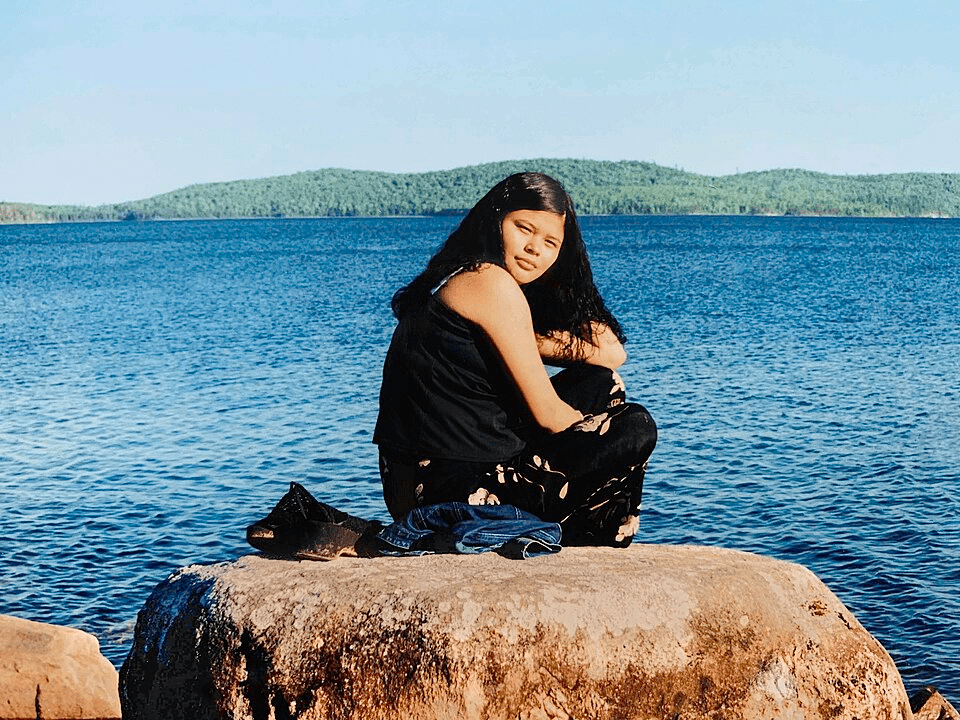
Chloe Bercovitz
News Editor
She told the nurses she was allergic to morphine.
Having endured severe stomach pain,she was admitted into hospital September 26th, 2020. Joyce Echequan, mother of seven, died due to the negligence of the attending nurses of Centre Hospitalier de Lanaudière.
Joyce Echequan’s heart problems kept her in and out of hospital for over five years, never fully trusting the medical staff. She was not fluent in French and would frequently live stream her visits on Facebook, for her sister to translate. On September 28th, 2020, she recorded some of the last moments of her life.
“According to CBC News, while in utter agony, Joyce was told that ‘she was only good for sex’ and ‘stupid as hell.‘ “
The nurses, prejudiced and racist, treated her as if she were a drug addict. A few hours later, Joyce Echequan died of pulmonary edema after having been administered morphine despite voicing her allergy.
Her death rattled the media during a time in which racism took centre-stage. The stories of George Floyd, and many others, became internationally known. During the lockdown, phones were filled with videos, statements, and promises for change; it seemed as if those in power had picked up this long-overdue call for justice. But now, it has been five years and the question remains: has the system changed?
In the past five years, this question has become a subject of growing research and reflection. The University of Waterloo, specifically, conducted a study exposing persistent racism in healthcare; a pattern that continues to fuel various, desperate appeals for justice and reform.
An anonymous participant of this study said, “I have been treated as though I would be a drug user trying to get meds to get high. My sister was treated the same way to the detriment of her health. She was in kidney failure and the medical personnel failed to treat this because they assumed that she was trying to get meds to abuse them.”
Thousands of Indigenous peoples in Canada report being stereotyped or seen as difficult. Numerous studies note a troubling precedent in which clinicians find the community either “unwilling to comply with treatment” or “uneducated about health issues.” There is so much irony in this frustration, given the role of healthcare professionals is oftentimes to provide such knowledge. Although, parents too, carry the nonsensical weight of being perceived as poor caregivers; many fear being apprehended by child protection agencies after hearing disparaging comments from medical personnel.
According to testimony taken from the Southern Chief’s Association, “Nurses at emergency thought I was only there for drugs when I thought I was having a heart attack. Paramedics thought I was on drugs when I was having a panic or angina attack. They kept badgering me to be honest; I kept telling them I wasn’t [lying]. They even took a test on me and didn’t tell me what they were doing. I finally went to hospital.”
According to Statistics Canada, precisely 50% of First Nations people experience discrimination and/or racism in a hospital emergency room.
Joyce Echequan’s death led to the creation of Joyce’s Principle, with her family hoping that her story would be met with tangible change. Embodying the foundation of Article 24 of the United Nations Declaration on the Rights of Indigenous Peoples (2007), it is, in essence, a call to action. In declaring internationally recognized rights, Joyce’s Principle serves as a reminder of the principles that various Canadian governments are to uphold. However, Jennifer Petiquay-Dufresne, the executive director of Joyce’s Principle Office, has made it very clear that it merely scratches the surface.
The minister responsible for First Nations and Inuit relations, Ian Lafrenière, has been consistently asked to comment on these issues. In reference to better implementation of Joyce’s Principle on a governmental scale, he stated that “the first criteria they asked from me is to recognize systemic racism. So, I’ll be honest, I’ll be straight and honest, it was impossible.” In saying so, he stressed that the province has been making changes. “It’s never going to [be] enough, to be honest. Why is that? [Because] you can’t catch up 400 years of history [just] like that,” said Lafrenière.
Such reforms boil down to two key elements: an optional Indigenous sensitivity training program available to health-care workers, and the addition of Bill 32 from 2024. This bill, which left First Nations groups unimpressed, established a “cultural safety approach within the health and social services network,” according to the National Assembly of Québec. They are merely the first steps of many, and critics worry that this has officials feeling as if their work is done.
Despite these efforts, First Nations communities are dissatisfied. While awareness has grown in recent years, instances of blatant racism and systemic, easily-preventable gaps persist. Candidly, acknowledgement alone is simply not enough.
“Truth and reconciliation cannot exclusively exist on paper.”
Until Indigenous peoples are safe, and until they receive the same level of medical care that any other patient would, the work of those in power remain unfinished.


Leave a comment